In the first of a two-part series, DR THOMAS GRAY describes the adrenaline rush and drama that a night in the trauma unit bring.
As medical professionals, it’s common to be asked about bizarre or exciting experiences. Undoubtedly, the tales with the best campfire credentials are the ones cultivated in the trauma unit. From the fast-paced, adrenaline-filled nights saving heavily injured patients from the brink of death, to the amusing results of a drunken escapade or the heart-wrenching reality of families and friends torn apart by tragedy – the trauma unit is an arena fraught with challenges, coupled with a conundrum of emotions.
For some, the blood, gore and chaos aren’t their cup of tea. For others, the adrenaline rush becomes an addiction. I grew up and went into medicine already captivated by images of what I thought it would be like to treat trauma patients, a possible a side effect of having watched the entire series of Chicago Hope.
South Africa has been recognised as having some of the highest rates of trauma in the world, contributing significantly to the burden of healthcare in the country. Most of this is due to motor vehicle accidents and interpersonal violence but many factors are believed to have contributed to this, including poverty, unequal socioeconomic circumstances and our history of apartheid.
We have some of the finest trauma facilities, both in public and in private, which are on par with international standards and we have so much trauma in SA that medical students and doctors from all over Europe, America and Australia travel to our hospitals in order to gain more experience treating trauma patients. They often confess that they would never have had this level of opportunity in their home countries. Some procedures routinely performed in our trauma units by students and junior doctors, and rarely seen overseas, would only be performed by senior doctors and specialists in developed countries. Here, trauma cases are so common that it’s imperative our doctors are trained to treat them early on.
For our homegrown doctors, trauma can be seen as a rite of passage. It’s almost impossible to pass through one’s training without having done a significant amount of trauma. It’s where we learn to throw our first few sutures (do stitches) and get used to inserting intravenous lines (put up drips). Once you’re more proficient and you move onto the more heavily injured patients, the vital skills of being able to think on your feet and work efficiently under pressure are nurtured.
Month-end heralds the much awaited paycheque for most people. For many South Africans, that means they have money to spend on alcohol – lots and lots of alcohol. By Saturday evening they’re so inebriated they wouldn’t recognise their best friends or siblings, much less their friends’ and siblings’ partners.
There are other factors that might cause a spike in trauma cases, namely: a Chiefs vs Pirates soccer match or a public holiday – specifically December 16 and New Year’s Day – and the weather. The former implies more drinking and more risky behaviour so you might be in for a chaotic call. As for the weather, rain tends to keep the alcoholics away but increases the number of trauma cases resulting from motor vehicle accidents.
As darkness descends, the daily frenzy present at most hospitals begins to settle. But this is when the trauma unit comes alive. The chaos is insidious as it approaches and reveals itself. The entrance doors suddenly slam open as a young man is dragged in by a group of friends, helped by a few security guards. The alarm bells in your head sound as you notice his blood-soaked clothes, although you can’t exactly see where it’s coming from and you are momentarily dazed by the intoxicating stench of alcohol for the first time that night. It won’t be the last.
You get the patient to an examination table and immediately a trauma team goes to work shouting orders and findings concurrently. While his airway is secured and oxygen administered, intravenous fluids are started. He’s found to have multiple stab wounds: chest, abdomen, right arm, left leg. His pulse is rapid and his blood pressure low; you get to work applying compression, trying to stop the bleeding. The team leader indicates that the patient has bleeding around the lung requiring a tube to be placed into his chest to drain the blood. You quickly volunteer. Wiping the sweat from your brow, trying to control your rapid breathing and your shaky hands, you successfully manage to get the tube inside him, much to your relief.
Once again the doors slam open with an almost identical scenario to the above. Again a trail of blood precedes that familiar, intoxicating smell of alcohol. The next trauma team goes to work on the patient. Suddenly there’s a scuffle in the middle of the room. It seems the friends of the two respective patients are getting into a heated argument.
Security fortunately steps in to restrain and remove them. You manage to speak to one of them outside to get the inside story. It’s usually quite predictable. The stab victims are close friends (sometimes brothers), once they were drunk enough, one of them made advances towards the other’s girlfriend, which resulted in the altercation and stabbings.
During a night in the trauma unit, it’s not uncommon to develop tunnel vision; your attention becomes focused on the emergency at hand. Only afterwards do you notice the slow but steady influx of patients piling up. The stench of alcohol becomes stronger, paralleled by the unmistakable smell of blood.
Eventually the scene resembles a mass trauma situation. Men lying all over and the occasional woman too. Some manage to sit, others are passed out on stretchers or strewn across the floor. Almost all are heavily intoxicated, bleeding from the characteristic jagged and irregular wounds made by broken bottles.
Next minute, the phone rings. A paramedic on scene is giving details of a family involved in a car accident. Your heart sinks as you listen to the report of the incoming patients and their injuries…
To be continued in part 2
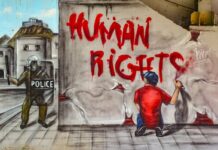
– Featured image via Wikimedia Commons
Dr Thomas Gray (*not his real name) is a doctor living (and slowly dying) inside a public hospital. He’s here to tell us what’s happening inside our hospitals. He would share his name with you, but then he’d have to kill you, and that would be unethical.
Enjoyed this piece? Help us to keep bringing you Dr Gray’s insights by donating to our crowdfunding campaign here.

![Trauma room [wikipedia]](https://www.thedailyvox.co.za/wp-content/uploads/2015/10/Trauma-room-wikipedia.jpg)